
FDA Approves Inotuzumab for Adults with B-Cell Acute Lymphoblastic Leukemia
September 18, 2017, by NCI Staff
The Food and Drug Administration (FDA) has approved inotuzumab ozogamicin (Besponsa®) for some adults with B-cell acute lymphoblastic leukemia (ALL).
The approval, announced on August 17, is for the use of inotuzumab in patients with B-cell ALL whose disease has stopped responding to (relapsed) or never responded to (refractory) standard chemotherapy.
Patients with B-cell ALL whose cancer has a specific genetic alteration known as the Philadelphia chromosome can receive inotuzumab only if their cancer has progressed despite treatment with one of several targeted drugs approved for this cancer type.
In the randomized phase 3 clinical trial on which the approval was based, called INO-VATE ALL, substantially more patients treated with inotuzumab had a complete remissioncompared with patients treated with chemotherapy. More patients in the inotuzumab group were also minimal residual disease (MRD) negative after treatment, meaning there was no evidence of leukemia cells present in the blood or bone marrow.
Patients in the trial treated with inotuzumab also had modest improvements in how long they lived without their disease progressing and in overall survival.
More Treatment Options for ALL
Although many patients with B-cell ALL respond well to chemotherapy, their cancer often returns. For patients with ALL whose cancer cells are positive for the Philadelphia chromosome—which occurs in 25% to 40% of cases—several targeted drugs, all part of a class of drugs known as tyrosine kinase inhibitors, have proven to be effective. But, as in patients treated with standard chemotherapy, the cancer develops resistance to the treatment and returns in many of these patients.
Inotuzumab is an antibody-drug conjugate, a type of drug in which an anticancer drug is chemically linked to another molecule that helps target the drug to cancer cells.
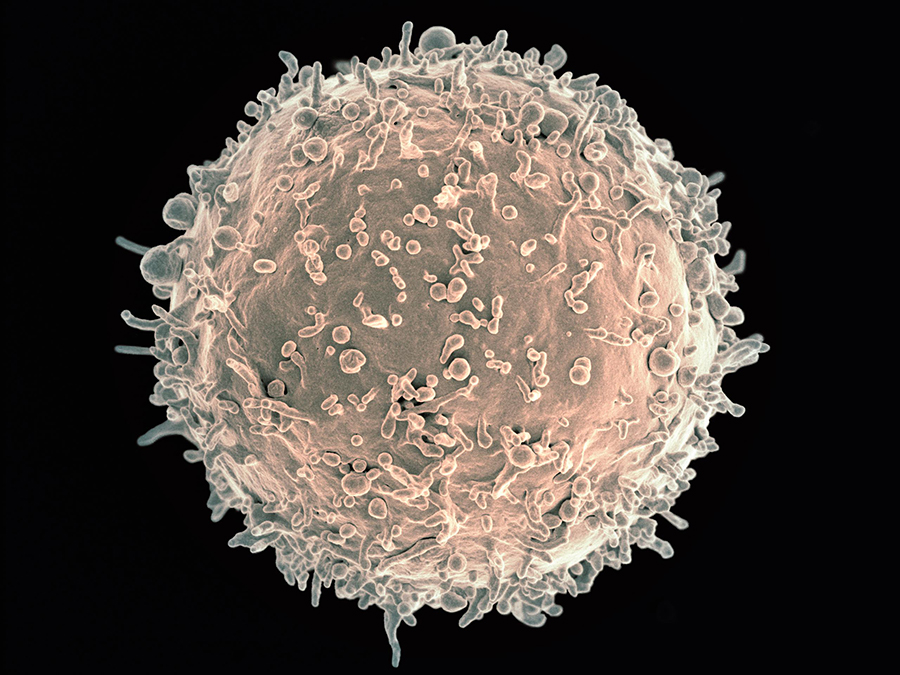
The targeting component of inotuzumab is a monoclonal antibody that targets the CD22 protein, which is produced in excess on the surface of most ALL cells. The antibody is linked to a compound called calicheamicin that kills cancer cells. Once the antibody portion of inotuzumab binds to CD22 on cancer cells, the calicheamicin is released into the cell, where it damages the cell’s DNA and causes its death.
Inotuzumab is the third new therapy approved in recent months for people with advanced B-cell ALL.
Earlier this year, FDA granted full approval of blinatumomab (Blincyto®), a form of immunotherapy, for children and adults with relapsed or refractory B-cell ALL regardless of Philadelphia chromosome status. The approval was based on the results of a large clinical trial showing that patients treated with the drug had substantial improvement in how long they lived compared with patients treated with chemotherapy.
And approximately 2 weeks after inotuzumab was approved, the agency approved tisagenlecleucel (Kymriah™), the first-ever approved CAR T-cell therapy, for children and young adults with advanced ALL. That approval was based on findings from a small clinical trial in which 83% of patients achieved a complete remission 3 months after receiving the treatment.
High Remission Rates with Inotuzumab
The more than 300 patients in the INO-VATE ALL trial—funded by Pfizer, the drug’s manufacturer—had received at least one chemotherapy regimen and, for those with Philadelphia chromosome–positive cancers, treatment with at least one FDA-approved tyrosine kinase inhibitor.
Of the first 218 patients in the trial (the group which served as the basis for the approval), approximately 36% of patients treated with inotuzumab had a complete remission, and nearly 90% of these patients were MRD negative. The complete remission and MRD-negative rates in patients treated with chemotherapy were approximately 17% and 32%, respectively.
Of the first 218 patients in the trial (the group which served as the basis for the approval), approximately 36% of patients treated with inotuzumab had a complete remission, and nearly 90% of these patients were MRD negative. The complete remission and MRD-negative rates in patients treated with chemotherapy were approximately 17% and 32%, respectively.
Among patients who achieved a complete remission, the median length of the responses was 8 months in those who received inotuzumab and 4.9 months in those who received chemotherapy.
The median progression-free survival in the trial was 5 months in patients treated with inotuzumab and 1.9 months in patients treated with chemotherapy. Median overall survival was 7.7 months and 6.7 months, respectively.
Common side effects of inotuzumab included infections, anemia, hemorrhage, and nausea. A nearly identical number of patients in both groups experienced serious side effects, with febrile neutropenia being the most frequently reported serious event.
Common side effects of inotuzumab included infections, anemia, hemorrhage, and nausea. A nearly identical number of patients in both groups experienced serious side effects, with febrile neutropenia being the most frequently reported serious event.
Treatment Decisions
The treatment goal for most patients with relapsed or refractory B-cell ALL is to respond well enough to their salvage therapy that they can go on to receive a potentially curative bone marrow transplant, explained Ryan Mattison, M.D., of the University of Wisconsin Carbone Cancer Center.
Inotuzumab now becomes “another option for trying to achieve remission or better disease control prior to transplant,” Dr. Mattison said.
In the INO-VATE ALL trial, he noted, 41% of patients who received inotuzumab were able to undergo a bone marrow transplant, compared with 11% who received standard chemotherapy.
For adults with ALL, the choice to use inotuzumab or blinatumomab may rely on different factors, Dr. Mattison said.
Blinatumomab, for instance, is given as a continuous infusion for 28 days. Because of this, “patients will need a central line and access to a pump, bag changes, and supportive nursing care during their treatment,” he said.
Inotuzumab, on the other hand, is given in a more traditional weekly schedule, which may be more convenient or practical for some patients, he added.
Patients’ other health conditions could also affect the choice, he noted. Because inotuzumab has a risk of liver-related side effects, a patient’s history of liver problems or of risk factors for them may play a role in the decision.
The approvals of inotuzumab and blinatumomab also set the stage for the possibility of using the drugs earlier in patients with B-cell ALL, Dr. Mattison said.
One NCI-sponsored clinical trial is already testing blinatumomab in combination with chemotherapy as an initial treatment for adults with B-cell ALL, and another NCI-sponsored trial is investigating the combination of inotuzumab and chemotherapy as an initial treatment in young adults with newly diagnosed B-cell ALL.
As for CAR T-cell therapy, under the approval for tisagenlecleucel, hospitals that want to offer this treatment must be specially certified. FDA explained that this certification includes special training for staff and other measures related to managing specific side effects of the treatment.





















.png)












No hay comentarios:
Publicar un comentario